Poor R Wave: Is It Always a Sign of Ischemia? Know Now!
Electrocardiography (ECG), a cornerstone of cardiac diagnostics, frequently presents with complex patterns requiring careful interpretation. Specifically, poor R wave progression, often observed in leads V1-V4, can raise concerns about underlying myocardial issues. The presence of a left anterior fascicular block, a type of intraventricular conduction delay, significantly influences the interpretation of these ECG findings, highlighting the need for comprehensive evaluation. Bayes’ Theorem provides a framework for understanding the pre-test probability and diagnostic accuracy of poor r wave progreession marker of ischemia in conjunction with other clinical indicators. Moreover, the American Heart Association (AHA) guidelines emphasize the importance of considering serial ECGs and clinical context to differentiate ischemic heart disease from other potential causes of abnormal R wave morphology.
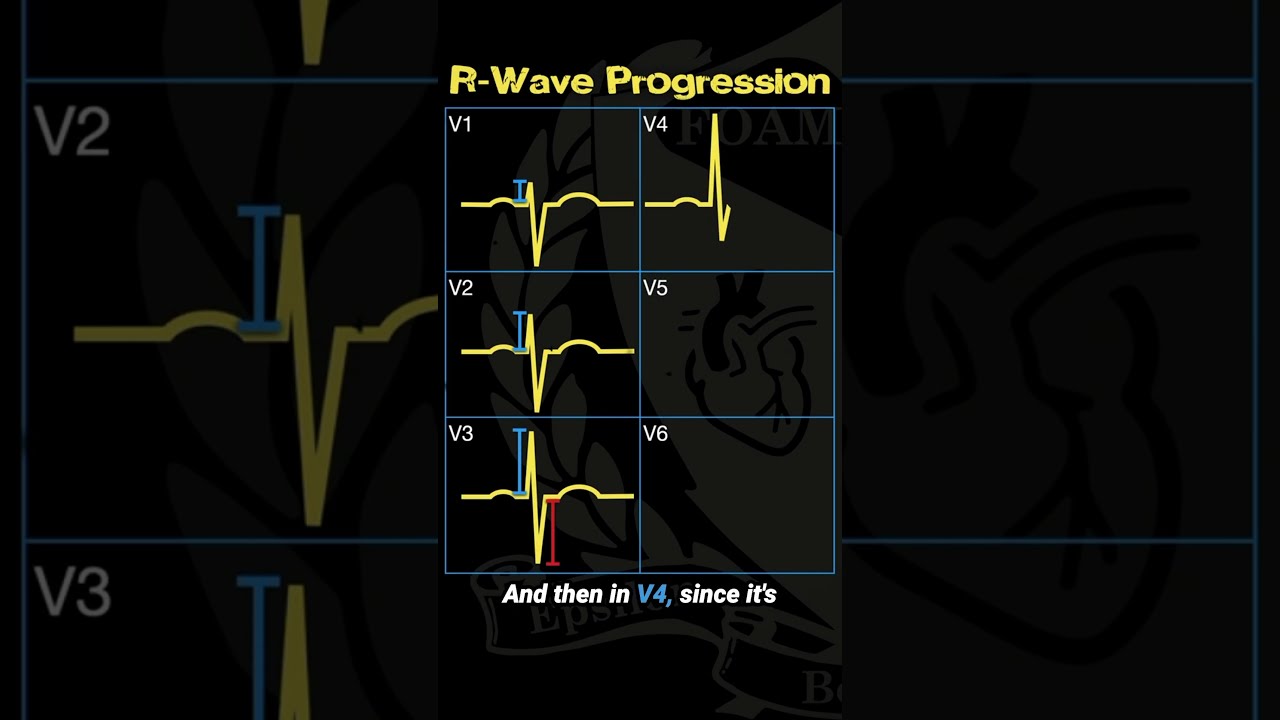
Image taken from the YouTube channel FOAMfrat Studios , from the video titled Understanding R Wave Progression .
Understanding Poor R Wave Progression and Its Significance in Ischemia
A concerning finding on an electrocardiogram (ECG), poor R wave progression (PRWP) can sometimes signal underlying heart problems. While frequently associated with myocardial ischemia, understanding its significance requires considering other potential causes. This article delves into the nuances of PRWP, focusing on its relationship with ischemia and exploring alternative explanations for its appearance.
What is Poor R Wave Progression?
Poor R wave progression refers to the abnormal increase in the R wave’s amplitude as you move from the right precordial leads (V1 and V2) to the left precordial leads (V5 and V6) on an ECG. Normally, the R wave should gradually become taller from V1 to V6, reflecting the increasing electrical activity moving towards the left ventricle. When this progressive increase is diminished or absent, it’s considered poor R wave progression.
Normal R Wave Progression: A Quick Reminder
- V1 & V2: Typically show a small R wave and a large S wave.
- V3 & V4: Transition zone, where the R and S wave amplitudes are roughly equal.
- V5 & V6: Predominantly large R waves with small or absent S waves.
Defining Poor R Wave Progression
Several criteria are used to define PRWP, though no single definition is universally accepted. Some common indicators include:
- R wave amplitude in V3 is less than 1.5mm.
- R wave in V3 is smaller than the R wave in V1 or V2.
- Absence of an R wave in V3.
- Persistent S wave in V6.
Poor R Wave Progression Marker of Ischemia: Exploring the Link
The association between PRWP and ischemia stems from the understanding that ischemia (reduced blood flow) can alter the electrical activity of the heart muscle. When a portion of the heart muscle is ischemic, it may not contribute effectively to the overall electrical activity detected by the ECG, leading to an attenuated R wave progression.
How Ischemia Affects R Wave Progression
- Decreased Myocardial Mass Contribution: Ischemic tissue may be electrically "silent" or contribute minimally, reducing the forward force during ventricular depolarization.
- Altered Conduction Pathways: Ischemia can disrupt the normal conduction pathways within the heart, affecting the sequence of ventricular activation and altering the ECG waveform.
- Scar Tissue Formation: Prior ischemic events can lead to scar tissue, which is electrically inactive and further impedes the normal R wave development.
ECG Changes Associated with Ischemia Beyond PRWP
It’s crucial to note that PRWP is rarely the sole indicator of ischemia. Other ECG changes that should be evaluated alongside PRWP include:
- ST-segment elevation or depression
- T-wave inversion
- Q waves (indicating prior myocardial infarction)
When Poor R Wave Progression Isn’t Ischemia: Other Potential Causes
While PRWP can be indicative of ischemia, numerous other factors can contribute to its appearance. A comprehensive evaluation is necessary to differentiate between ischemic and non-ischemic causes.
Non-Ischemic Cardiac Causes
- Left Ventricular Hypertrophy (LVH): Increased left ventricular mass can affect the electrical axis and alter R wave progression. However, LVH usually presents with other distinct ECG features (e.g., increased QRS voltage, ST-segment depression and T-wave inversion in lateral leads).
- Bundle Branch Blocks: Conduction delays in either the left or right bundle branch can significantly alter ventricular depolarization and affect R wave progression. Specifically, a left bundle branch block (LBBB) classically causes PRWP.
- Cardiomyopathies: Conditions affecting the heart muscle, such as dilated or hypertrophic cardiomyopathy, can disrupt the electrical activity and influence R wave progression.
- Wolff-Parkinson-White (WPW) Syndrome: This pre-excitation syndrome can alter the conduction pathway and affect the QRS complex morphology, potentially masking or altering R wave progression.
Non-Cardiac Causes
-
Technical Errors: Improper electrode placement is a common cause of artifactual PRWP. This includes both high and low placement of chest leads.
- Solution: Careful re-assessment of lead placement and repeating the ECG is important for any interpretation of PRWP.
- Chronic Obstructive Pulmonary Disease (COPD): Lung hyperinflation can alter the heart’s position in the chest, affecting the ECG recording and potentially mimicking PRWP.
- Chest Wall Deformities: Scoliosis or pectus excavatum can alter the heart’s electrical axis and affect the ECG waveform.
- Obesity: Excessive chest wall thickness can dampen the electrical signals, leading to an apparent reduction in R wave amplitude.
- Age: The prevalence of PRWP increases with age, even in the absence of ischemic heart disease.
A Table Summarizing Differential Diagnoses
| Cause | Description | Associated ECG Findings |
|---|---|---|
| Myocardial Ischemia | Reduced blood flow to the heart muscle. | ST-segment changes, T-wave inversion, Q waves. |
| Left Ventricular Hypertrophy | Increased left ventricular mass. | Increased QRS voltage, ST-segment depression, T-wave inversion in lateral leads. |
| Left Bundle Branch Block | Conduction delay in the left bundle branch. | Widened QRS complex, absence of Q waves in lateral leads, ST-segment and T-wave changes discordant with QRS. |
| COPD | Lung hyperinflation. | Low voltage, right axis deviation. |
| Electrode Misplacement | Improper placement of ECG electrodes. | May mimic other conditions; repeating the ECG with correct placement usually resolves the abnormality. |
Diagnostic Approach to Poor R Wave Progression
A finding of poor R wave progression on an ECG requires a careful and methodical approach to determine its underlying cause. The diagnostic process should involve:
- Reviewing the Patient’s Clinical History: Assess risk factors for coronary artery disease (e.g., hypertension, diabetes, smoking, family history), presence of chest pain or other cardiac symptoms, and history of prior cardiac events.
- Careful ECG Interpretation: Evaluating the ECG for other signs of ischemia or other cardiac abnormalities (e.g., LVH, bundle branch block). Confirming the absence of lead misplacement.
- Further Investigations: If ischemia is suspected, further testing such as cardiac stress testing (e.g., exercise ECG, stress echocardiogram, nuclear stress test) or coronary angiography may be necessary. If non-ischemic causes are suspected, echocardiography or other relevant investigations may be considered.
FAQs: Understanding Poor R Wave Progression
Here are some common questions about poor R wave progression, its significance, and how it relates to ischemia.
What exactly does "poor R wave progression" mean on an EKG?
Poor R wave progression refers to the gradual increase in R wave amplitude from lead V1 to V6 being absent or diminished. Ideally, the R wave should become taller as you move from V1 to V6. If it doesn’t, it’s considered poor R wave progression.
Does poor R wave progression always mean I’m having a heart attack?
No, poor R wave progression does not always indicate a heart attack. While it can be a marker of ischemia or a previous heart attack, other conditions like lung disease, left ventricular hypertrophy, or incorrect electrode placement can also cause it. Further testing is usually needed.
So, if it’s not always ischemia, what else should I worry about with poor R wave progression?
Besides acute ischemia, poor r wave progreession marker of ischemia can also be a chronic sign related to prior myocardial infarction (heart attack). Structural heart changes and even normal variants might be the cause. Your doctor will consider your medical history and other EKG findings to determine the most likely cause.
What’s the next step if my EKG shows poor R wave progression?
Further investigation is crucial. Your doctor will likely order additional tests, such as cardiac enzymes (to rule out a heart attack), an echocardiogram (to assess heart structure and function), or a stress test. These tests will help determine if poor r wave progreession marker of ischemia is linked to any critical cardiac issue.
So, next time you hear about a poor r wave progreession marker of ischemia, remember there’s more to the story! Keep asking questions, and stay informed!