Pleural Fluid Lymphocytes: The Ultimate Guide!
Pleural effusions, abnormal accumulations of fluid in the pleural space, often necessitate diagnostic evaluation. The cellular composition of this fluid, particularly the presence of lymphocytes, plays a crucial role in discerning the underlying etiology. Pleural fluid lymphocytes, therefore, become a key focus in understanding conditions ranging from tuberculosis to malignancy. A comprehensive analysis of pleural fluid lymphocytes helps guide clinicians in accurately diagnosing and managing pleural diseases. This guide explores these aspects in detail.
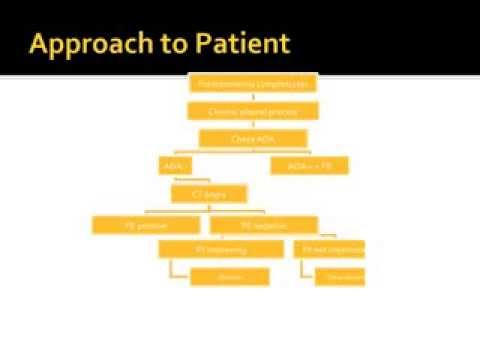
Image taken from the YouTube channel ICUCorner , from the video titled Interpretation of Pleural Effusion Analysis .
Deconstructing the Ideal Article Layout: "Pleural Fluid Lymphocytes: The Ultimate Guide!"
To create a comprehensive and informative article on "Pleural Fluid Lymphocytes," the layout should prioritize clarity, accessibility, and a logical progression of information. The following outline provides a suggested structure:
1. Introduction: Setting the Stage
- Briefly define pleural fluid: Begin by explaining what pleural fluid is and its normal function in the pleural space (the space between the lungs and the chest wall). Emphasize its lubricating role.
- Introduce lymphocytes: Define lymphocytes as a type of white blood cell integral to the immune system.
- Connect pleural fluid and lymphocytes: Clearly state that lymphocytes can be found within pleural fluid.
- Highlight the article’s purpose: Clearly articulate that the guide will explore the significance of pleural fluid lymphocytes, including their normal levels, elevated levels, causes, and diagnostic implications. This section should intrigue the reader and establish the article’s value.
2. Understanding Pleural Fluid Analysis (Thoracentesis)
- Explain thoracentesis: Detail the process of thoracentesis – a medical procedure to collect pleural fluid. Explain the steps involved, including preparation and post-procedure care.
- Purpose of fluid analysis: Explain why pleural fluid is analyzed. Highlight that one aspect of this analysis involves assessing the number and types of cells present, including lymphocytes.
- Safety considerations: Briefly mention common risks associated with thoracentesis, reassuring readers that the procedure is generally safe when performed by qualified professionals.
3. Lymphocytes: A Closer Look
-
Types of Lymphocytes: Describe the major types of lymphocytes (T cells, B cells, and Natural Killer cells) and their individual roles in the immune response. A table might be helpful here:
Lymphocyte Type Primary Function T Cells Cell-mediated immunity; directly killing infected cells; regulating immune responses. B Cells Producing antibodies to neutralize pathogens. NK Cells Killing infected or cancerous cells without prior sensitization. -
Lymphocyte Activation: Briefly explain how lymphocytes are activated when they encounter antigens (foreign substances). This lays the foundation for understanding why their numbers might increase in pleural fluid.
4. Normal Levels of Pleural Fluid Lymphocytes
- Defining the "normal" range: Provide a typical reference range for lymphocyte count in pleural fluid. It’s important to specify the units (e.g., cells/µL or percentage of total cells).
- Factors affecting normal values: Acknowledge that "normal" can vary slightly based on laboratory and individual patient factors.
- Clinical Significance of normal findings: Emphasize that a normal level doesn’t always rule out disease; it simply suggests that lymphocytes aren’t significantly contributing to any abnormalities in the pleural space at the time of testing.
5. Elevated Pleural Fluid Lymphocytes (Lymphocytosis)
- Defining Lymphocytosis: Explicitly define what constitutes lymphocytosis in the context of pleural fluid. This might differ from lymphocytosis in blood.
- Common Causes of Pleural Fluid Lymphocytosis: Detail the most frequent causes of an elevated lymphocyte count in pleural fluid. This section should be broken down further.
5.1. Infections
- Tuberculosis (TB): Explain the strong association between pleural fluid lymphocytosis (especially T-cell predominance) and TB pleurisy.
- Viral Infections: Describe how viral infections can also trigger lymphocyte accumulation in the pleural space.
5.2. Malignancy
- Lymphoma: Explain how lymphoma (cancer of the lymphatic system) can involve the pleura, leading to high lymphocyte counts.
- Metastatic Cancer: Discuss how cancer that has spread to the pleura from elsewhere in the body (e.g., lung, breast) can stimulate an immune response and increase lymphocyte levels.
5.3. Autoimmune Diseases
- Rheumatoid Arthritis (RA): Explain the link between RA and pleural effusions characterized by lymphocytosis.
- Systemic Lupus Erythematosus (SLE): Describe how SLE can cause pleural inflammation and lymphocyte accumulation.
5.4. Other Causes
- Sarcoidosis: Detail how this inflammatory disease can affect the pleura and result in increased lymphocyte levels.
- Chylothorax: Explain how leakage of lymphatic fluid into the pleural space (chylothorax) will naturally increase the number of lymphocytes.
- Diagnostic Workup for Lymphocytosis: Explain that elevated pleural fluid lymphocytes are not a diagnosis in themselves. Detail the additional tests and procedures that might be necessary to determine the underlying cause (e.g., pleural biopsy, imaging studies, further fluid analysis).
6. Interpreting Pleural Fluid Lymphocyte Results
- Linking Results to Clinical Context: Explain how lymphocyte counts are interpreted alongside other findings from the pleural fluid analysis (e.g., total protein, glucose, LDH, cell types) and the patient’s medical history and symptoms.
- Additional Tests: Mention other tests that might be performed to further characterize the lymphocytes, such as flow cytometry (to identify specific lymphocyte subtypes) and cytology (to look for malignant cells).
7. Managing Conditions Associated with Pleural Fluid Lymphocytosis
- General Management Principles: Briefly outline the general approaches to managing conditions that cause pleural fluid lymphocytosis. The specific treatment will depend entirely on the underlying cause (e.g., antibiotics for TB, chemotherapy for lymphoma, immunosuppressants for autoimmune diseases).
- Role of Pleurodesis: Briefly mention pleurodesis as a procedure that can prevent fluid buildup in the pleural space if the effusion is recurrent and difficult to manage.
FAQs: Understanding Pleural Fluid Lymphocytes
This FAQ section addresses common questions about pleural fluid lymphocytes to help you better understand their significance.
What does a high level of lymphocytes in pleural fluid indicate?
A high level of lymphocytes in the pleural fluid often suggests an inflammatory or infectious process. Tuberculosis and malignancy are common causes. Further investigation is usually needed to determine the specific cause and guide treatment.
Can benign conditions cause elevated pleural fluid lymphocytes?
Yes, benign conditions can sometimes lead to increased pleural fluid lymphocytes. Examples include autoimmune diseases, reactions to medications, and post-cardiac injury syndrome. The overall clinical picture is important in diagnosis.
How are pleural fluid lymphocytes measured and analyzed?
Pleural fluid lymphocytes are typically measured as part of a complete pleural fluid analysis. The fluid is collected via thoracentesis and sent to a lab. The lab counts the different types of cells present, including lymphocytes, to determine their percentage.
Why is it important to analyze pleural fluid lymphocytes?
Analyzing pleural fluid lymphocytes helps differentiate between various causes of pleural effusions (fluid buildup around the lungs). Knowing the lymphocyte count, along with other test results, helps doctors accurately diagnose and treat the underlying condition affecting the lungs.
So, that’s the lowdown on pleural fluid lymphocytes! Hopefully, this gave you a clearer picture. Dive deeper as needed, and good luck out there!