PICC Line Blood Draws: Safe or Risky? Find Out!
The Peripheral Inserted Central Catheter (PICC), a type of central venous catheter, is frequently utilized for long-term medication administration. However, a common question arises concerning its versatility: can bloods be drawn through a PICC line safely and effectively? Understanding the guidelines from organizations like the Infusion Nurses Society (INS) is paramount when considering this procedure. The decision often hinges on factors such as the patient’s specific clinical situation and the skill of the registered nurse performing the blood draw. Exploring these aspects sheds light on the potential benefits and risks associated with obtaining blood samples via PICC lines, impacting patient care within hospital settings.
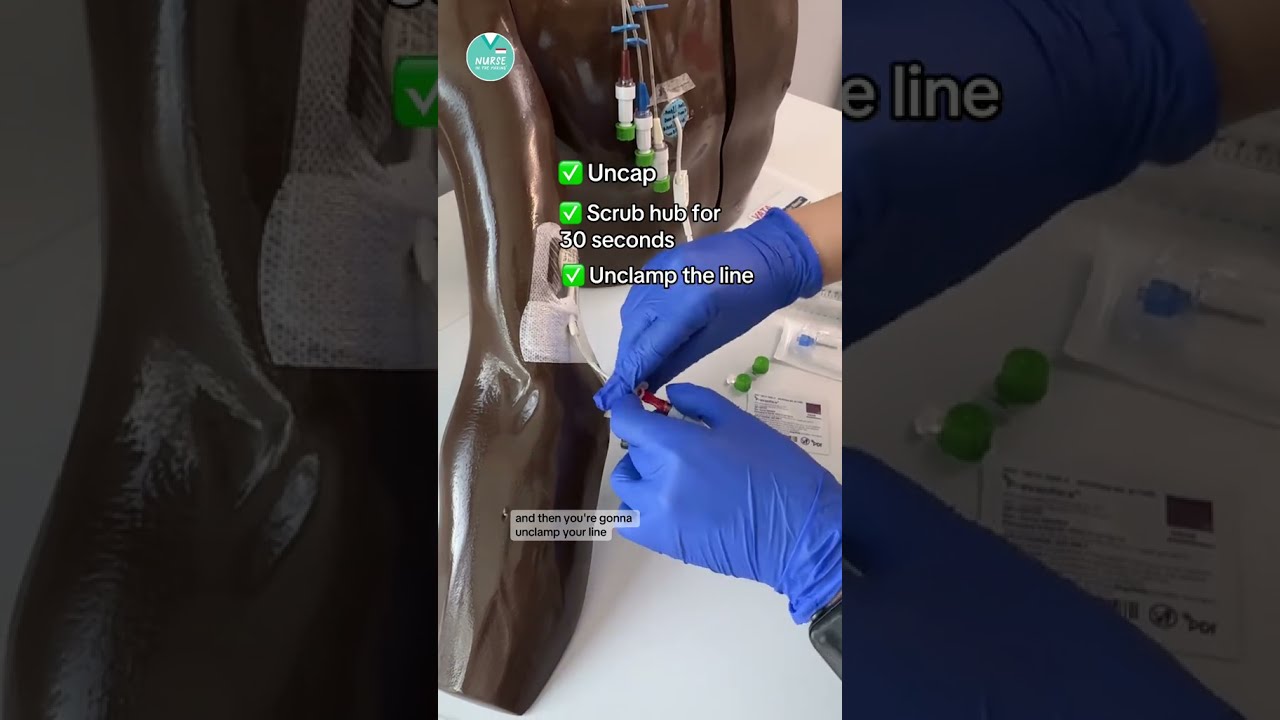
Image taken from the YouTube channel NurseInTheMaking , from the video titled 🩸How to draw labs from a PICC or CVC #RN #BSN #futurenurse .
PICC Line Blood Draws: Safe or Risky?
The use of Peripherally Inserted Central Catheters, or PICC lines, has become increasingly common in modern healthcare. These long, thin catheters are inserted into a peripheral vein, typically in the arm, and advanced until the tip reaches a large vein near the heart.
PICC lines offer a convenient and reliable method for delivering medications, fluids, and nutrition directly into a patient’s bloodstream over an extended period. However, their utility extends beyond administration.
One area of ongoing debate and clinical consideration revolves around the practice of drawing blood through PICC lines.
PICC Lines: A Brief Overview
A PICC line is a type of central venous catheter used for patients requiring long-term intravenous therapy.
It’s inserted by a trained healthcare professional, often a nurse or physician, using ultrasound guidance to navigate the catheter into the appropriate vein.
The placement is confirmed with an X-ray. Common uses include delivering antibiotics, chemotherapy, and total parenteral nutrition (TPN).
Patients who require frequent blood draws or have difficult venous access often benefit from PICC line placement, as it reduces the need for repeated needle sticks.
The Central Question: Phlebotomy via PICC – Is it Safe?
The central question that guides this discussion is: Can blood draws (phlebotomy) be performed through a PICC line safely?
While seemingly convenient, drawing blood from a PICC line is not without its potential complications.
The practice introduces a unique set of risks and benefits that must be carefully weighed.
Balancing Risks and Benefits: A Preliminary Look
The potential benefits of drawing blood through a PICC line include increased patient comfort, reduced venipunctures, and decreased risk of extravasation (leakage of fluid into surrounding tissues).
However, these benefits must be carefully balanced against the potential risks, such as infection, thrombosis (blood clot formation), catheter occlusion (blockage), and damage to the catheter itself.
These risks can have significant consequences for patient health and well-being.
Therefore, a thorough understanding of both the advantages and disadvantages is essential for making informed clinical decisions regarding PICC line blood draws.
The previous section laid the groundwork for understanding the central question surrounding PICC lines and blood draws. Now, to fully address the complexities of this debate, it’s essential to delve deeper into the specifics of what a PICC line is, how it functions, and the patient populations for whom it is most beneficial.
What is a PICC Line? A Detailed Explanation
A Peripherally Inserted Central Catheter (PICC line) is a long, thin, flexible tube inserted into a peripheral vein, usually in the upper arm, and advanced until its tip reaches a large vein in the chest, near the heart. This allows for reliable access to the central venous system.
Insertion and Placement
The insertion procedure is typically performed by a trained healthcare professional, such as a registered nurse or physician, who has received specialized training in PICC line placement. Ultrasound guidance is generally used to visualize the veins and facilitate accurate insertion, minimizing the risk of complications.
After insertion, the position of the PICC line is confirmed with a chest X-ray to ensure that the tip is correctly located in the superior vena cava or cavoatrial junction. This confirmation is crucial for ensuring the safe and effective delivery of medications and fluids.
Common Uses of PICC Lines
PICC lines are widely used in various clinical settings for patients requiring long-term intravenous therapy. Their primary purpose is to provide a reliable and convenient route for administering medications, fluids, and nutritional support directly into the bloodstream.
Some common uses of PICC lines include:
-
Antibiotic Administration: Prolonged courses of intravenous antibiotics for treating serious infections.
-
Chemotherapy: Delivery of chemotherapy drugs for cancer treatment.
-
Total Parenteral Nutrition (TPN): Providing complete nutritional support to patients unable to eat or absorb nutrients adequately through their digestive system.
-
Pain Management: Administration of pain medications for chronic pain conditions.
-
Fluid Replacement: Long-term fluid replacement therapy for patients with dehydration or electrolyte imbalances.
Patient Populations Requiring PICC Lines
PICC lines are particularly beneficial for patients who require frequent or prolonged intravenous therapy and/or those with difficult venous access. The following are some common patient populations who may require a PICC line:
-
Cancer Patients: Undergoing chemotherapy or requiring long-term supportive care.
-
Patients with Chronic Infections: Requiring extended courses of intravenous antibiotics.
-
Patients with Gastrointestinal Disorders: Needing TPN due to malabsorption or bowel dysfunction.
-
Patients with Chronic Kidney Disease: Requiring frequent hemodialysis or other intravenous treatments.
-
Patients with Poor Venous Access: Those with a history of difficult IV starts or collapsed veins.
By providing reliable and consistent vascular access, PICC lines can significantly improve patient comfort, reduce the need for repeated needle sticks, and enhance the overall quality of care.
The previous section laid the groundwork for understanding the central question surrounding PICC lines and blood draws. Now, to fully address the complexities of this debate, it’s essential to delve deeper into the specifics of what a PICC line is, how it functions, and the patient populations for whom it is most beneficial.
The PICC Line Blood Draw Debate: Advantages and Considerations
The question of whether drawing blood through a PICC line is a generally accepted practice within the medical community is far from straightforward. While PICC lines are primarily intended for medication and fluid administration, the practice of drawing blood through them remains a topic of discussion, influenced by varying institutional policies, clinical guidelines, and individual patient needs.
Accepted Practice or Contentious Issue?
The acceptance of drawing blood from PICC lines varies significantly across healthcare settings. Some institutions have established protocols and training programs that support the practice, viewing it as a valuable tool for reducing patient discomfort and minimizing venipunctures.
Conversely, other facilities discourage or outright prohibit blood draws from PICC lines due to concerns about potential complications and the availability of alternative blood-drawing methods. This divergence in practice highlights the need for standardized guidelines and comprehensive risk-benefit assessments.
Patient-Centric Advantages of PICC Line Blood Draws
One of the most compelling arguments in favor of drawing blood through PICC lines revolves around patient comfort. For individuals requiring frequent blood tests, repeated venipunctures can be a source of considerable pain, anxiety, and vein damage.
A PICC line offers a convenient and less traumatic alternative, eliminating the need for multiple needle sticks and preserving peripheral veins. This can be especially beneficial for patients with chronic illnesses, fragile veins, or those receiving long-term intravenous therapy.
Furthermore, drawing blood through a PICC line can streamline the blood collection process, reducing the time and resources required for phlebotomy. This can improve efficiency in busy clinical settings and minimize disruptions to patient care.
Counterarguments: Safety and Potential Complications
Despite the potential benefits, concerns regarding safety and potential complications remain central to the debate surrounding PICC line blood draws. The primary worry revolves around the increased risk of infection, particularly central line-associated bloodstream infections (CLABSI), which can have severe consequences for patients.
Drawing blood through a PICC line can also increase the risk of thrombosis (blood clot formation) and catheter occlusion (blockage), both of which can compromise the line’s functionality and necessitate costly interventions. Additionally, there is a risk of damaging the catheter during the blood draw procedure, potentially leading to further complications.
Ultimately, the decision of whether to draw blood through a PICC line requires a careful balancing of potential benefits and risks, taking into account individual patient factors, institutional policies, and the availability of alternative blood-drawing methods.
The advantages of PICC line blood draws, particularly concerning patient comfort and reduced venipunctures, are certainly compelling. However, a balanced perspective requires a thorough examination of the potential downsides. Understanding the risks associated with this practice is crucial for informed decision-making and safe implementation.
Unveiling the Risks: Potential Complications of PICC Line Blood Draws
While PICC lines offer undeniable benefits, the practice of drawing blood from them is not without potential complications. These risks must be carefully considered and mitigated through strict adherence to best practices.
Infection: A Primary Concern
One of the most significant risks associated with any central line, including PICC lines, is infection. Drawing blood provides an additional opportunity for bacteria to enter the bloodstream, potentially leading to serious complications.
Central Line-Associated Bloodstream Infections (CLABSI) are a major concern in healthcare settings, associated with increased morbidity, mortality, and healthcare costs. While not solely caused by blood draws, the procedure can contribute to the risk if proper sterile technique is not meticulously followed.
Localized infections at the insertion site are also possible, presenting with redness, swelling, pain, or discharge. Prompt recognition and treatment of these infections are crucial to prevent them from progressing to more serious bloodstream infections.
Thrombosis: The Risk of Blood Clots
Thrombosis, or blood clot formation, is another significant risk associated with PICC lines, and drawing blood can exacerbate this. The presence of a foreign object like a catheter within a blood vessel naturally increases the risk of clot formation.
Drawing blood can disrupt blood flow and potentially damage the inner lining of the vein, further promoting clot development. These clots can partially or completely block the PICC line, rendering it unusable.
Furthermore, clots can dislodge and travel to other parts of the body, leading to more serious complications such as pulmonary embolism or deep vein thrombosis (DVT).
Catheter Occlusion: Maintaining Patency
Catheter occlusion, or blockage of the PICC line, is a common problem that can be caused or worsened by drawing blood. When blood is drawn, particularly if the line is not adequately flushed afterwards, blood can remain within the catheter and clot, leading to partial or complete blockage.
Occlusion prevents the delivery of medications and fluids and necessitates further intervention to restore patency, potentially requiring the use of thrombolytic agents or even PICC line removal and replacement.
Other Potential Complications
In addition to the risks outlined above, other less common but still significant complications can arise from drawing blood through PICC lines. These include:
- Catheter Damage: Improper technique during blood draw attempts can potentially damage the catheter itself, leading to leaks, cracks, or breaks.
- Phlebitis: Inflammation of the vein surrounding the PICC line can occur, causing pain, redness, and swelling.
- Air Embolism: Although rare, air can be introduced into the bloodstream during the blood draw procedure if proper technique is not followed.
Understanding these potential risks is essential for healthcare providers to make informed decisions about whether drawing blood through a PICC line is the most appropriate course of action for a particular patient. Furthermore, it reinforces the critical need for strict adherence to best practices and protocols to minimize these risks and ensure patient safety.
The risks associated with PICC line blood draws are real and demand respect. However, these risks can be significantly mitigated through strict adherence to established protocols and a commitment to best practices. Ensuring patient safety and maintaining the integrity of the PICC line itself are paramount, requiring a multi-faceted approach encompassing technique, knowledge, and vigilance.
Safety First: Best Practices for PICC Line Blood Draws
Drawing blood from a PICC line should never be a routine procedure, but rather a carefully considered act performed with precision and unwavering attention to detail. Safe and successful blood draws through PICC lines hinge on a foundation of rigorous protocols, skilled practitioners, and a culture of safety within the healthcare setting.
The Collaborative Roles of Nurses and Physicians
Both nurses and physicians play crucial, yet distinct, roles in ensuring the safety of PICC line blood draws. Nurses, often at the forefront of patient care, are typically responsible for the hands-on procedure, requiring a deep understanding of PICC line maintenance, sterile technique, and potential complications.
Physicians contribute by establishing clear orders for blood draws, considering the appropriateness of using the PICC line versus peripheral venipuncture, and managing any complications that may arise. This collaboration ensures that the procedure is both necessary and performed with the highest level of care.
Adherence to Established Guidelines
Several professional organizations, including the Infusion Nurses Society (INS) and the Centers for Disease Control and Prevention (CDC), offer comprehensive guidelines for PICC line maintenance and blood draws. These guidelines serve as the cornerstone of safe practice, providing evidence-based recommendations on everything from insertion site care to flushing protocols.
Strict adherence to these guidelines is not optional; it is a fundamental requirement for minimizing the risk of infection, thrombosis, and other complications. Healthcare facilities must ensure that all staff members involved in PICC line care are thoroughly trained and competent in following these recommendations.
The Imperative of Sterile Technique
The importance of sterile technique cannot be overstated. Any breach in sterility during the blood draw procedure creates an opportunity for bacteria to enter the bloodstream, potentially leading to a Central Line-Associated Bloodstream Infection (CLABSI).
This necessitates the use of sterile gloves, drapes, and instruments, as well as meticulous hand hygiene before, during, and after the procedure. Furthermore, the insertion site must be thoroughly cleansed with an appropriate antiseptic solution.
Antiseptic Measures: Chlorhexidine’s Role
Chlorhexidine-based antiseptics are generally considered the gold standard for skin antisepsis prior to accessing a PICC line. These solutions have been proven to be highly effective in reducing the number of bacteria on the skin, thereby minimizing the risk of infection.
The antiseptic should be applied using a friction scrub technique, allowing sufficient contact time to maximize its antimicrobial effect. It is crucial to allow the antiseptic to dry completely before accessing the PICC line.
Maintaining Blood Sample Quality
Drawing blood from a PICC line can sometimes compromise sample quality due to factors such as catheter dead space and the potential for hemolysis. To mitigate these issues, a discard volume of blood should be drawn and discarded prior to collecting the sample for analysis.
This discard volume removes any residual fluids or medications that may be present in the catheter, ensuring that the sample accurately reflects the patient’s blood composition. Proper labeling and handling of the blood sample are also essential to maintain its integrity.
Flush Solutions: Preventing Catheter Occlusion
Appropriate flushing of the PICC line after blood draws is critical to prevent catheter occlusion. Both saline and heparin solutions are commonly used for flushing, with the choice depending on institutional protocols and patient-specific factors.
Saline is effective for removing blood and debris from the catheter lumen, while heparin may be used to prevent clot formation, particularly in patients at high risk for thrombosis. The flushing technique should involve a pulsatile or turbulent flow to maximize the removal of any residual material.
Drawing blood from a PICC line, when executed with precision and adherence to protocol, can offer significant benefits. However, it’s equally crucial to recognize that not all situations are conducive to this practice. Understanding when not to draw blood from a PICC line is just as important as knowing how to do it safely.
Contraindications: When Drawing Blood from a PICC Line is Inadvisable
While PICC lines offer a convenient route for blood sampling, certain circumstances render their use for this purpose either unsafe or inappropriate. Identifying these contraindications is paramount to patient safety and PICC line maintenance.
Compromised PICC Line Integrity
Any sign of structural damage to the PICC line itself is a definitive contraindication.
This includes, but is not limited to:
- Visible cracks or breaks in the catheter.
- Leaks around the insertion site.
- Kinks or bends in the catheter that impede flow.
Attempting to draw blood through a compromised PICC line risks further damage, potentially leading to catheter rupture, embolism, or extravasation of fluids.
Suspected Infection at the Insertion Site
The presence of any signs of infection near the PICC line insertion site should immediately preclude its use for blood draws.
Such signs may include:
- Redness or swelling.
- Purulent drainage.
- Localized pain or tenderness.
- Elevated local skin temperature.
Drawing blood through an infected PICC line introduces the risk of bacteremia or sepsis, severely compromising the patient’s health. The possibility of a Central Line-Associated Bloodstream Infection (CLABSI) is significantly heightened.
Visible Signs of Thrombosis
Evidence of thrombus formation, either within the PICC line itself or in the surrounding vasculature, is another critical contraindication.
This might manifest as:
- Swelling or pain in the arm where the PICC line is inserted.
- Visible distension of veins in the arm or chest.
- Difficulty flushing the PICC line.
Attempting a blood draw in the presence of a thrombus can dislodge the clot, leading to a pulmonary embolism or further vascular compromise.
Patient-Specific Risk Factors
Certain patient-specific conditions can also increase the risks associated with PICC line blood draws, warranting caution or outright contraindication.
These include:
- Coagulation Disorders: Patients with known bleeding disorders or those receiving anticoagulant therapy may be at increased risk of bleeding or hematoma formation.
- Thrombocytopenia: Low platelet counts can increase the risk of bleeding complications.
- Renal Insufficiency: Some flush solutions (e.g., heparin) may be contraindicated or require dose adjustment in patients with impaired renal function.
- Allergies: Known allergies to antiseptics or flush solutions must be carefully considered.
In these situations, alternative methods of blood collection should be strongly considered to minimize potential harm to the patient. Always consult with a physician before proceeding with a PICC line blood draw in the presence of these risk factors.
Drawing blood from a PICC line, when executed with precision and adherence to protocol, can offer significant benefits. However, it’s equally crucial to recognize that not all situations are conducive to this practice. Understanding when not to draw blood from a PICC line is just as important as knowing how to do it safely.
With so much hinging on appropriate technique and patient selection, where does the ultimate responsibility lie for ensuring PICC lines are managed correctly, and that blood draws are only performed when safe and indicated? The answer, inevitably, rests with the healthcare facilities themselves.
Healthcare Facilities’ Role in PICC Line Management
Healthcare facilities, including hospitals, clinics, and long-term care centers, bear a significant responsibility in ensuring the proper management of PICC lines. This encompasses everything from initial insertion and routine maintenance to blood draw protocols and prompt intervention when complications arise. A facility’s commitment to standardized protocols and ongoing education is paramount to patient safety and positive outcomes.
Establishing Comprehensive PICC Line Protocols
The foundation of effective PICC line management lies in the establishment of comprehensive, evidence-based protocols. These protocols must address all aspects of PICC line care, including:
-
Insertion Guidelines: Standardized procedures for insertion, including site selection, sterile technique, and confirmation of catheter placement.
-
Maintenance Protocols: Clear guidelines for routine flushing, dressing changes, and assessment of the insertion site.
-
Blood Draw Procedures: Detailed instructions on proper technique for drawing blood, including the use of appropriate supplies, minimizing catheter manipulation, and post-draw flushing.
-
Complication Management: Protocols for recognizing and managing potential complications, such as infection, thrombosis, and catheter occlusion.
These protocols should be readily accessible to all healthcare providers involved in PICC line care, and they should be regularly reviewed and updated to reflect current best practices.
Implementing and Enforcing Guidelines
Establishing protocols is only the first step. Healthcare facilities must also actively implement and enforce these guidelines to ensure consistent adherence across all departments and personnel. This requires a multi-faceted approach that includes:
-
Education and Training: Providing comprehensive education and training to all nurses, physicians, and other healthcare providers involved in PICC line care. This training should cover all aspects of PICC line management, including insertion, maintenance, blood draw techniques, and complication management.
-
Competency Assessment: Regularly assessing the competency of healthcare providers in performing PICC line procedures. This can be accomplished through observation, skills checklists, and written examinations.
-
Auditing and Monitoring: Implementing a system for auditing and monitoring adherence to PICC line protocols. This can involve regular chart reviews, direct observation of procedures, and data analysis to identify areas for improvement.
-
Standardized Supplies: Ensuring that all healthcare providers have access to the necessary supplies and equipment for safe and effective PICC line care. This includes appropriate catheters, sterile dressings, antiseptics, and flush solutions.
Fostering a Culture of Safety
Ultimately, the success of PICC line management depends on fostering a culture of safety within the healthcare facility. This involves creating an environment where healthcare providers feel empowered to speak up about concerns, report errors, and actively participate in quality improvement initiatives.
-
Open Communication: Encouraging open communication and collaboration among all members of the healthcare team. This includes creating opportunities for nurses, physicians, and other healthcare providers to share their experiences, ask questions, and provide feedback on PICC line protocols.
-
Just Culture: Adopting a "just culture" approach to error reporting, where mistakes are viewed as opportunities for learning and improvement, rather than as grounds for punishment. This encourages healthcare providers to report errors without fear of reprisal, which can help to identify systemic problems and prevent future incidents.
-
Patient Involvement: Actively involving patients in their own PICC line care. This includes educating patients about the purpose of their PICC line, how to care for it, and what signs and symptoms to watch out for. By empowering patients to take an active role in their care, healthcare facilities can improve adherence to protocols and reduce the risk of complications.
By prioritizing comprehensive protocols, diligent implementation, and a strong safety culture, healthcare facilities can significantly enhance the safety and efficacy of PICC line blood draws and overall PICC line management, ultimately leading to better patient outcomes.
PICC Line Blood Draws: Your Questions Answered
Got questions about PICC line blood draws after reading our article? Here are some answers to frequently asked questions to help clarify the process and its potential risks.
Is it always safe to draw blood from a PICC line?
While PICC lines are designed for medication administration and blood draws, it’s not always completely risk-free. Following proper technique and adhering to strict sterile protocols are essential to minimize risks like infection or damage to the catheter. When these protocols are followed, bloods can be drawn through a PICC line safely.
What are the main risks associated with drawing blood from a PICC line?
The most common risks include infection at the insertion site or within the bloodstream, clotting within the catheter, and damage to the PICC line itself, potentially leading to its malfunction or requiring replacement. Careful handling and maintenance are vital to prevent these complications.
Why draw blood from a PICC line instead of a regular vein?
PICC lines are often used for patients needing frequent blood tests, long-term IV medications, or those with difficult-to-access veins. Using a PICC line reduces the need for repeated needle sticks, minimizing discomfort and potential vein damage. If bloods can be drawn through a PICC line, it simplifies the blood collection process.
What happens if a PICC line becomes blocked during or after a blood draw?
If a PICC line becomes blocked, a trained healthcare professional will attempt to flush it with a special solution to dissolve the clot. If that doesn’t work, medications to break down the clot might be required, or in some cases, the PICC line might need to be replaced. Prevention through proper flushing and maintenance is key.
So, after weighing the ins and outs, what’s the verdict on whether can bloods be drawn through a picc line? Hopefully, you’ve got a clearer picture now. Always best to chat with your healthcare team to figure out what’s right for you! Take care!