Hysterectomy & Hiatal Hernia: Is There a Link? Find Out!
The question of can a hysterectomy cause a hiatal hernia is one that often arises when discussing women’s health. A hysterectomy, a surgical procedure involving the removal of the uterus, represents a significant intervention. The diaphragm, a crucial muscle for breathing, also plays a role in the development of hiatal hernias, and its anatomy can be impacted by various factors. This relationship is further examined within the context of gastroesophageal reflux disease (GERD), a condition frequently associated with hiatal hernias. Understanding the connection between these elements involves consulting with healthcare providers such as gastroenterologists to determine the likelihood of a correlation.
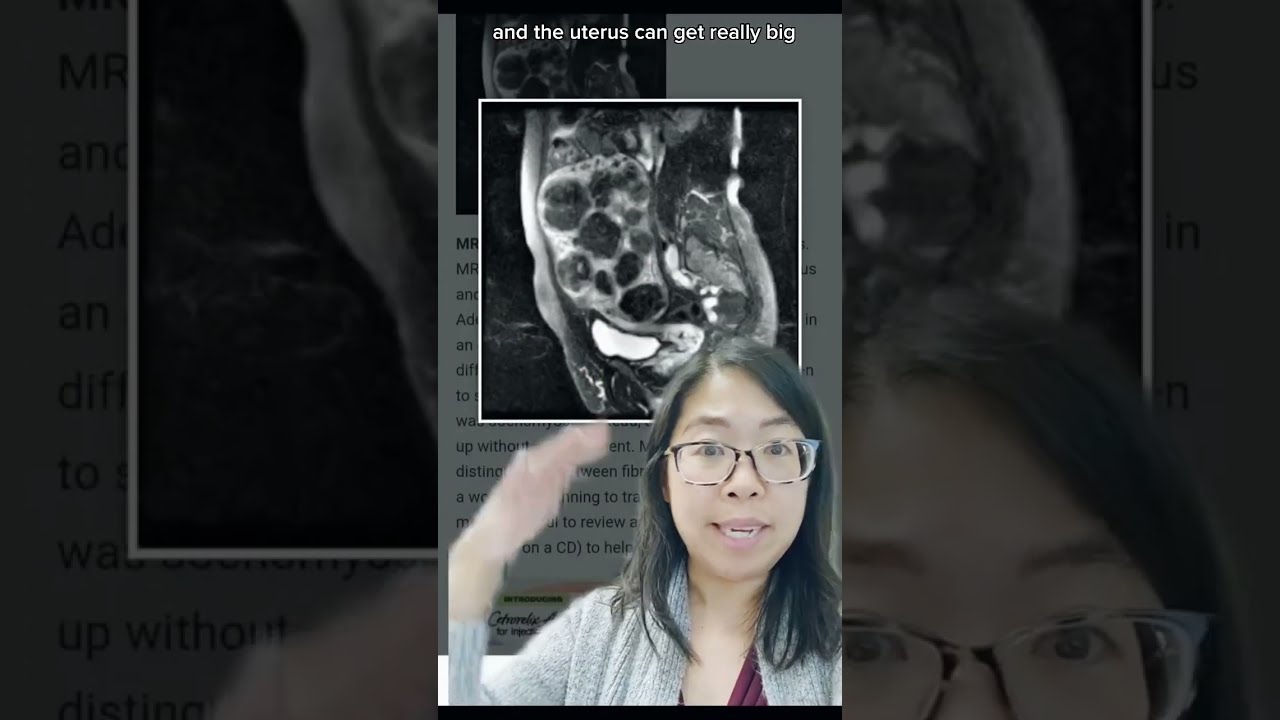
Image taken from the YouTube channel Karen Tang, MD , from the video titled What happens to the *space* where the uterus was after a HYSTERECTOMY? Gynecologist Explains! #short .
Women’s health is a complex tapestry, woven with interconnected threads. Among the many factors influencing well-being, two conditions, hysterectomy and hiatal hernia, often arise as points of concern and require careful consideration. A hysterectomy involves the surgical removal of the uterus. A hiatal hernia occurs when a portion of the stomach protrudes through the diaphragm.
Both conditions can significantly impact a woman’s quality of life. Understanding their individual effects is the first step in addressing a question that has lingered in the minds of many: can a hysterectomy lead to a hiatal hernia?
Hysterectomy and Hiatal Hernia: A Brief Overview
Let’s briefly explore each condition to set the stage for understanding their potential relationship.
Understanding Hysterectomy
A hysterectomy, the surgical removal of the uterus, is a significant procedure often recommended for various reasons, including:
- Fibroids
- Endometriosis
- Uterine prolapse
- Certain cancers
The impact of a hysterectomy extends beyond the reproductive system, influencing hormonal balance and potentially affecting other bodily functions.
Understanding Hiatal Hernia
A hiatal hernia involves the protrusion of a part of the stomach through the diaphragm, the muscle separating the chest and abdomen. This condition can lead to:
- Heartburn
- Acid reflux
- Discomfort
Risk factors like obesity, age, and increased intra-abdominal pressure contribute to its development.
The Central Question: Can a Hysterectomy Cause a Hiatal Hernia?
The core question we aim to address is: Can a hysterectomy cause a hiatal hernia? This is not a question with a straightforward yes or no answer. It requires a nuanced exploration of potential mechanisms and contributing factors.
Understanding this potential connection is crucial for:
- Informed decision-making
- Proactive management
- Improved patient care
By examining the potential links, we empower women and healthcare providers to make informed choices and manage health proactively.
Addressing Concerns and Anxieties
It’s natural to feel concerned or anxious when considering the potential connections between surgical procedures and other health conditions. Rest assured, you are not alone in seeking clarity.
This exploration aims to provide a balanced perspective, acknowledging both the potential risks and the available evidence. Our goal is to offer information that empowers you to have informed conversations with your healthcare providers, addressing your specific concerns and anxieties with knowledge and confidence.
The question of whether a hysterectomy can cause a hiatal hernia is complex, and we’ll delve into potential mechanisms later. To fully understand the possible connection, it’s crucial to first establish a firm understanding of each condition individually. Let’s begin by exploring the intricacies of a hysterectomy, a procedure that can significantly impact a woman’s life.
Understanding Hysterectomy: A Detailed Overview
A hysterectomy is a surgical procedure involving the removal of the uterus.
It’s a significant medical intervention with lasting consequences, so understanding the procedure itself, the reasons behind it, and its potential effects on the body is essential.
What is a Hysterectomy?
At its core, a hysterectomy is the surgical removal of the uterus, the central organ of the female reproductive system responsible for menstruation and pregnancy.
The procedure effectively ends a woman’s ability to conceive and carry a child.
Different types of hysterectomies exist, each varying in the extent of tissue removed:
-
Partial Hysterectomy: Only the uterus is removed, leaving the cervix intact.
-
Total Hysterectomy: The entire uterus, including the cervix, is removed. This is the most common type of hysterectomy.
-
Radical Hysterectomy: The uterus, cervix, upper part of the vagina, and surrounding tissues (including lymph nodes) are removed. This is typically performed in cases of cancer.
The surgical approach also varies. Here’s a quick look:
Types of Hysterectomy Procedures
-
Abdominal Hysterectomy: The uterus is removed through an incision in the abdomen. This method typically requires a longer recovery period.
-
Vaginal Hysterectomy: The uterus is removed through an incision in the vagina. This approach usually results in a shorter recovery time.
-
Laparoscopic Hysterectomy: The uterus is removed using small incisions in the abdomen with the aid of a laparoscope (a thin, lighted tube with a camera). This is a minimally invasive approach.
-
Robot-Assisted Laparoscopic Hysterectomy: Similar to laparoscopic hysterectomy, but a robotic system is used to enhance precision and control.
The choice of procedure depends on various factors, including the reason for the hysterectomy, the size of the uterus, and the patient’s overall health.
Why is a Hysterectomy Performed?
A hysterectomy is not a first-line treatment. It is usually considered when other less invasive options have been explored or are deemed unsuitable.
Several conditions may lead a doctor to recommend a hysterectomy:
-
Uterine Fibroids: These noncancerous tumors can cause heavy bleeding, pain, and pressure on the bladder or bowel.
-
Endometriosis: This condition causes the uterine lining to grow outside the uterus, leading to pain, irregular bleeding, and infertility.
-
Uterine Prolapse: This occurs when the uterus sags or drops into the vagina, often due to weakened pelvic floor muscles.
-
Abnormal Uterine Bleeding: Persistent, heavy, or irregular bleeding that doesn’t respond to other treatments may necessitate a hysterectomy.
-
Adenomyosis: This condition occurs when the uterine lining grows into the muscular wall of the uterus, causing pain and heavy bleeding.
-
Cancer: Hysterectomy may be part of the treatment plan for cancers of the uterus, cervix, or ovaries.
It is important to remember that a hysterectomy is a major surgical decision that should be made in consultation with a healthcare professional after careful consideration of all available options.
Potential Effects on the Body
Beyond the immediate surgical recovery, a hysterectomy can have lasting effects on a woman’s body, both physically and emotionally.
One of the most significant consequences is the cessation of menstruation and the inability to become pregnant.
Hormonal Impact
The removal of the uterus can also disrupt hormonal balance, especially if the ovaries are removed during the procedure (oophorectomy).
The ovaries are the primary source of estrogen and progesterone in women. Removal of ovaries can lead to:
-
Menopause: If the ovaries are removed before natural menopause, it can trigger surgical menopause, leading to symptoms like hot flashes, vaginal dryness, and mood swings.
-
Hormone Therapy: Hormone replacement therapy (HRT) may be prescribed to manage these symptoms.
Impact on Other Organs
Even when the ovaries are conserved, there can still be hormonal shifts.
Additionally, the removal of the uterus can impact other organs and systems in the body.
Changes in pelvic floor strength and bladder function are commonly reported.
The potential impact on the bowel and its potential implications for conditions like hiatal hernia are areas requiring further investigation.
Understanding these potential effects is crucial for women considering a hysterectomy. It allows them to be prepared for the changes they may experience and to discuss management strategies with their healthcare providers.
Having explored the intricacies of a hysterectomy, it’s equally important to understand the other key player in our discussion: the hiatal hernia. Let’s unravel the details of this condition, exploring its causes, risk factors, and telltale symptoms.
Understanding Hiatal Hernia: Causes, Risk Factors, and Symptoms
A hiatal hernia occurs when the upper part of your stomach bulges through the diaphragm, a large muscle separating your abdomen and chest.
The diaphragm has a small opening (hiatus) through which your esophagus passes before connecting to your stomach.
In a hiatal hernia, the stomach pushes up through that opening and into your chest cavity.
What Exactly is a Hiatal Hernia?
Essentially, a hiatal hernia is a structural abnormality.
Normally, the diaphragm acts as a barrier, keeping the stomach safely tucked away in the abdomen.
When this barrier weakens, or the opening enlarges, the stomach can start to creep upwards.
The Esophagus’s Role
The esophagus is the tube that carries food and liquids from your mouth to your stomach.
It passes through the diaphragm via the hiatus.
When a hiatal hernia is present, the normal relationship between the esophagus, the diaphragm, and the stomach is disrupted.
This disruption can lead to various symptoms, as we’ll discuss later.
Risk Factors: Who’s More Likely to Develop a Hiatal Hernia?
Several factors can increase your risk of developing a hiatal hernia.
While anyone can develop this condition, certain populations are more susceptible.
Obesity is a significant risk factor, as excess weight can put increased pressure on the abdomen.
Age also plays a role, as the diaphragm can weaken over time.
Increased intra-abdominal pressure, regardless of the cause, can contribute.
This can occur from:
- Chronic coughing
- Straining during bowel movements
- Heavy lifting
Recognizing the Signs: Common Symptoms
Many people with small hiatal hernias experience no symptoms at all.
These hernias are often discovered incidentally during tests for other conditions.
However, larger hiatal hernias can cause a range of uncomfortable symptoms.
Heartburn and acid reflux are among the most common.
This occurs because the hernia allows stomach acid to flow back up into the esophagus.
Difficulty swallowing, also known as dysphagia, can also occur.
Other potential symptoms include:
- Chest pain
- Belching
- Feeling unusually full after eating
- Vomiting blood or passing black stools (rare, but can indicate bleeding).
Having explored the intricacies of a hysterectomy, it’s equally important to understand the other key player in our discussion: the hiatal hernia. Let’s unravel the details of this condition, exploring its causes, risk factors, and telltale symptoms.
Exploring the Link: How Hysterectomy Might Relate to Hiatal Hernia
This section delves into the heart of the matter: could a hysterectomy be a contributing factor to the development of a hiatal hernia?
It’s a question that warrants careful consideration, as the interplay between surgical procedures, anatomical structures, and physiological changes is complex.
Let’s explore the potential connections, examining the evidence and acknowledging the uncertainties.
The Central Question: Can a Hysterectomy Cause a Hiatal Hernia?
The direct answer, based on current research, is complex and often inconclusive.
While a definitive causal relationship hasn’t been firmly established, there are plausible mechanisms through which a hysterectomy could potentially influence the development or exacerbation of a hiatal hernia.
It’s crucial to understand that correlation does not equal causation.
Further research is needed to fully elucidate the nature and strength of any association between these two conditions.
The Role of Intra-abdominal Pressure
One of the primary areas of investigation revolves around intra-abdominal pressure (IAP).
This refers to the pressure within the abdominal cavity, which is normally regulated by a delicate balance of muscle activity and organ positioning.
Impact of Abdominal and Pelvic Floor Changes
A hysterectomy, by its very nature, involves significant changes to the abdominal and pelvic anatomy.
The removal of the uterus can alter the support structures within the pelvis, potentially impacting the function of the abdominal muscles and pelvic floor muscles.
These muscles play a vital role in maintaining IAP and supporting the abdominal organs.
If these muscles weaken or their function is compromised following a hysterectomy, it could lead to an increase in IAP.
This increase in pressure could then, theoretically, contribute to the development or worsening of a hiatal hernia by pushing the stomach upwards through the diaphragm.
Intra-abdominal Pressure and Hiatal Hernia Development
Elevated IAP can place undue stress on the diaphragm, the muscle that separates the chest cavity from the abdomen.
As previously discussed, the diaphragm has a small opening, the hiatus, through which the esophagus passes.
Sustained or repeated increases in IAP could weaken the tissues around the hiatus, making it easier for the stomach to push through and create a hiatal hernia.
Factors like chronic coughing, straining during bowel movements, and obesity can also raise IAP and compound the potential risk.
Hormonal Changes and Their Impact
Beyond the structural changes, hormonal shifts following a hysterectomy might also play a role.
Estrogen’s Influence
Estrogen, a key hormone produced by the ovaries, has a multifaceted impact on the body.
After a hysterectomy, particularly one involving the removal of the ovaries (oophorectomy), estrogen levels can decline significantly.
This hormonal shift can potentially influence muscle strength and tissue elasticity, including the muscles of the diaphragm and the tissues surrounding the hiatus.
Some studies suggest that reduced estrogen levels may contribute to muscle weakness and decreased tissue integrity, which could indirectly increase the susceptibility to a hiatal hernia.
It’s important to note that the precise mechanisms by which hormonal changes might affect hiatal hernia development are still being investigated.
Evidence from Studies/Research
The existing body of research on the direct link between hysterectomy and hiatal hernia is limited.
Some studies have suggested a possible association, while others have found no significant correlation.
This inconsistency in findings highlights the need for more robust and comprehensive research in this area.
It’s essential to approach the available evidence with a critical eye, acknowledging the limitations of individual studies.
Acknowledging Limitations
Many studies are retrospective, meaning they look back at past events, which can introduce biases.
Sample sizes may be small, and confounding factors, such as age, obesity, and other medical conditions, may not be adequately controlled for.
Furthermore, the diagnostic criteria for hiatal hernia can vary, making it difficult to compare results across different studies.
Therefore, while the existing research provides some clues, it’s crucial to interpret the findings cautiously and recognize the need for further investigation to clarify the nature and strength of any potential link between hysterectomy and hiatal hernia.
Having explored the potential connections between hysterectomy and hiatal hernia, it’s time to shift our focus towards proactive measures. What can be done, both from a medical perspective and through personal choices, to mitigate the risk or manage the symptoms? Let’s delve into the insights offered by experts and explore practical strategies for prevention.
Expert Insights and Preventative Strategies
Gynecological Perspectives on Hysterectomy Decisions
The decision to undergo a hysterectomy is rarely taken lightly. Gynecologists carefully weigh various factors before recommending this procedure.
These factors include the severity of the patient’s condition, her overall health, her age, and her desire for future childbearing.
When considering a hysterectomy, gynecologists often assess the potential impact on surrounding organs and tissues.
While the primary focus is on addressing the uterine issue, skilled surgeons are mindful of minimizing disruption to the abdominal and pelvic floor.
They take steps to preserve the integrity of these structures, which can indirectly influence intra-abdominal pressure.
The type of hysterectomy performed (e.g., laparoscopic, vaginal, abdominal) can also impact recovery and potential long-term effects. Gynecologists carefully select the most appropriate surgical approach based on the individual patient’s anatomy and medical history.
Lifestyle Modifications for Risk Management
Beyond surgical considerations, lifestyle modifications play a crucial role in managing risk factors associated with hiatal hernia, especially after a hysterectomy.
These changes can significantly impact intra-abdominal pressure and overall well-being.
Weight Management
Maintaining a healthy weight is paramount. Excess weight, particularly abdominal fat, increases intra-abdominal pressure, potentially exacerbating or contributing to a hiatal hernia.
A balanced diet rich in fiber, fruits, and vegetables can promote healthy weight management and reduce the strain on the abdominal cavity.
Strengthening Abdominal Muscles
Strengthening abdominal muscles can provide support to the core and help regulate intra-abdominal pressure.
However, it’s crucial to engage in exercises that don’t excessively strain the abdomen.
Consulting with a physical therapist or qualified fitness professional can help design a safe and effective exercise program.
Exercises like planks, gentle core engagement, and diaphragmatic breathing can be beneficial.
Avoid exercises that involve heavy lifting or straining, as these can increase intra-abdominal pressure.
Dietary Adjustments
Dietary adjustments can also help manage symptoms associated with hiatal hernia, such as heartburn and acid reflux.
Avoiding trigger foods, such as caffeine, alcohol, spicy foods, and fatty foods, can reduce the frequency and severity of these symptoms.
Eating smaller, more frequent meals can also prevent overfilling the stomach and reduce pressure on the diaphragm.
Posture and Breathing
Maintaining good posture can help reduce pressure on the abdomen. Sitting and standing upright allows for better organ alignment and reduces the risk of compression.
Practicing diaphragmatic breathing (belly breathing) can help strengthen the diaphragm and improve overall respiratory function.
This type of breathing can also help reduce stress and promote relaxation, which can indirectly benefit digestive health.
Hysterectomy & Hiatal Hernia: FAQs
Here are some frequently asked questions regarding the potential link between hysterectomy and hiatal hernias. We aim to clarify any uncertainties you may have.
What exactly is a hiatal hernia?
A hiatal hernia occurs when part of your stomach bulges up through an opening in your diaphragm and into your chest. This opening is where your esophagus normally passes through. It can cause symptoms like heartburn and acid reflux.
Is there a proven direct cause-and-effect relationship between hysterectomy and hiatal hernia?
Currently, there’s no conclusive scientific evidence that directly links hysterectomy to causing hiatal hernias. While some studies explore possible indirect connections, it’s not a guaranteed outcome. Other risk factors often play a more significant role.
If no direct link, why is this connection sometimes discussed?
The connection is often discussed because hysterectomies involve abdominal surgery, which can potentially impact core muscle strength and intra-abdominal pressure. These factors can sometimes influence the development or worsening of a hiatal hernia, but this is not definitively proven. One might also wonder, can a hystorectomy cause a hiatal hernia in predisposed women? The answer is that it may possibly increase the risk slightly in some individuals, but other factors are more significant.
What factors are more commonly associated with hiatal hernia development?
Common risk factors for hiatal hernia include obesity, aging, smoking, heavy lifting, and persistent coughing. Genetics and congenital conditions can also contribute. Managing these lifestyle factors can often play a larger role in preventing or mitigating hiatal hernia symptoms than whether or not someone has undergone a hysterectomy.
So, there you have it! Hopefully, you now have a clearer picture of whether a hysterectomy can cause a hiatal hernia. As always, chat with your doctor if you’re concerned – they’re the real experts! Take care!