Post-Hysterectomy Cycle Tracker: What Happens to Your Body?
Understandably, many women wonder about changes to their bodies after a hysterectomy. The uterus, responsible for menstruation, is removed during this procedure, often leading women to ask: is there a cycle tracker for post hysterectomy? The answer isn’t always straightforward. Hormonal fluctuations can still occur even without a uterus, particularly if the ovaries remain. These hormonal shifts might lead some women to seek ways of monitoring potential symptoms, even if traditional menstruation ceases. Further adding to these complex changes is the possibility of pelvic pain, which can influence the perception of a ‘cycle’ despite the absence of uterine bleeding.
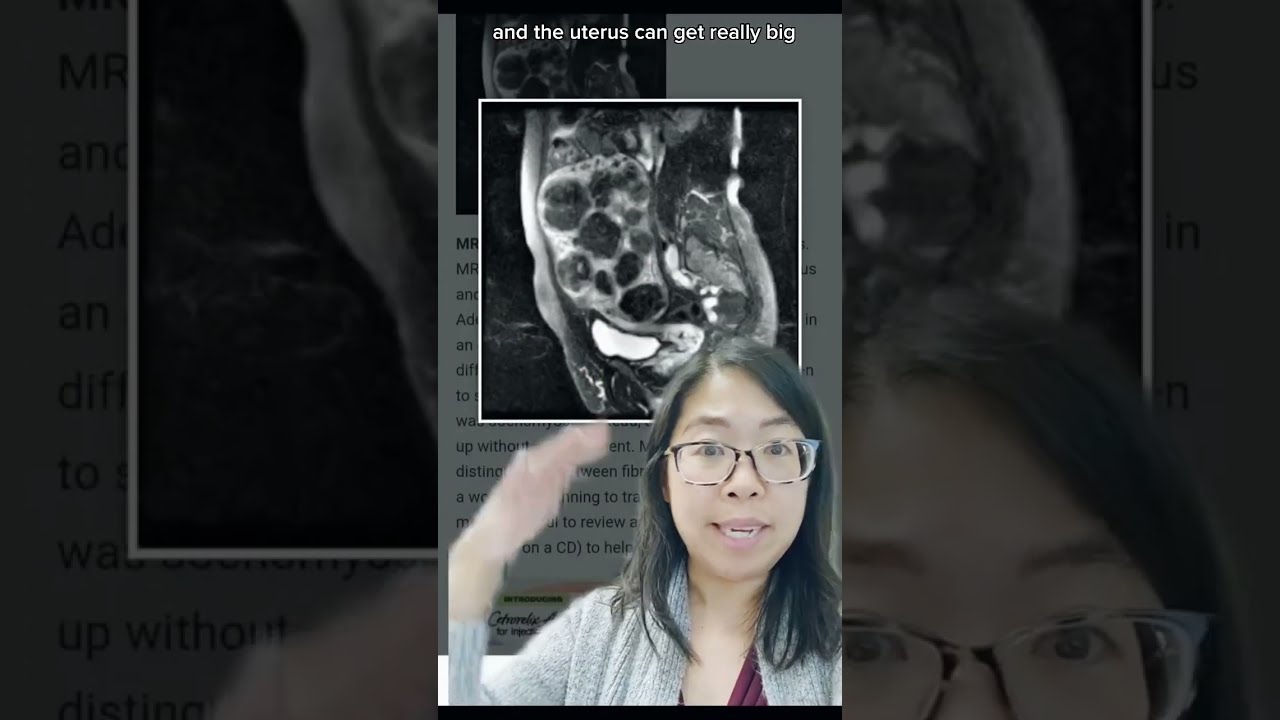
Image taken from the YouTube channel Karen Tang, MD , from the video titled What happens to the *space* where the uterus was after a HYSTERECTOMY? Gynecologist Explains! #short .
Is There a Cycle Tracker for Post-Hysterectomy? Understanding Changes After Surgery
Many women wonder about their cycles after a hysterectomy. It’s a natural question! This article addresses whether a cycle tracker is relevant after a hysterectomy and explains the bodily changes you might experience.
Why Track a Cycle? The Role of Hormones
Before diving into post-hysterectomy scenarios, let’s quickly recap why women track their cycles in the first place.
- Hormonal Fluctuations: Tracking helps understand the ebb and flow of hormones like estrogen and progesterone.
- Fertility Awareness: Knowing your cycle is essential for family planning.
- Symptom Monitoring: Tracking can reveal patterns related to PMS, mood swings, and other cyclical symptoms.
- Identifying Irregularities: Cycle tracking helps detect unusual patterns that might warrant a doctor’s visit.
What Happens During a Hysterectomy?
A hysterectomy involves the surgical removal of the uterus. Different types of hysterectomies exist, and the organs removed vary:
- Partial Hysterectomy: Only the uterus is removed. The cervix is left in place.
- Total Hysterectomy: Both the uterus and cervix are removed.
- Radical Hysterectomy: The uterus, cervix, upper part of the vagina, and surrounding tissues are removed. This is typically done in cases of cancer.
- Hysterectomy with Oophorectomy: One or both ovaries are removed in addition to the uterus.
The type of hysterectomy significantly impacts what you can expect afterward.
Is There a Cycle Tracker for Post-Hysterectomy?
The direct answer is: usually no. After a complete hysterectomy (uterus and cervix removed), you will no longer have menstrual periods. The lining of the uterus, which sheds during menstruation, is gone. However, the necessity and use of a tracker depend heavily on whether the ovaries were removed.
Ovaries Still Present:
If your ovaries were not removed (ovaries are preserved), you will not have menstrual bleeding, but your ovaries will likely continue to produce hormones. You may experience symptoms related to hormonal fluctuations. In this case:
- Possible Symptom Tracking: You might choose to track symptoms like mood changes, hot flashes, or vaginal dryness, which could be related to the cyclical production (or sometimes erratic production) of hormones.
- Focus Shift: Instead of tracking bleeding, you’d track any symptoms and their intensity.
- Use of a Tracker: While a "cycle tracker" specifically designed for menstruation isn’t necessary, a general symptom tracker (even a notebook!) can be helpful to monitor these changes and discuss them with your doctor. You could use a menstrual cycle tracker, but manually ignore the bleeding section.
Ovaries Removed: Surgical Menopause
If your ovaries were removed (oophorectomy), you’ll likely enter surgical menopause. This means:
- No More Hormones Produced: The ovaries no longer produce significant amounts of estrogen and progesterone.
- No Cyclical Fluctuations: Because there are significantly reduced or no hormonal fluctuations, there is no longer a cyclical hormonal pattern to track.
- Focus on Managing Menopausal Symptoms: The focus shifts to managing menopausal symptoms, such as hot flashes, night sweats, vaginal dryness, and mood changes. These symptoms may be constant or intermittent, but not tied to a cycle.
- Tracker Irrelevance: A cycle tracker is not relevant in this scenario. Tracking focuses on the severity and frequency of menopausal symptoms, rather than predicting a cycle.
Understanding Post-Hysterectomy Symptoms
Regardless of whether your ovaries were removed, it’s important to understand potential post-hysterectomy symptoms.
Hormonal Changes (Ovaries Still Present):
Even if your ovaries remain, they may not function exactly as they did before surgery. They could become less efficient in hormone production. Some women report continued cyclic symptoms with less intensity.
Hormonal Changes (Ovaries Removed):
You will experience a more abrupt hormonal change. Symptoms can include:
- Hot flashes and night sweats
- Vaginal dryness
- Sleep disturbances
- Mood swings and irritability
- Decreased libido
- Bone density loss
Non-Hormonal Changes:
Regardless of whether your ovaries were removed, you might also experience:
- Changes in bladder or bowel function
- Pelvic pain
- Scar tissue formation
- Emotional adjustments
Alternative Tracking Methods for Symptom Management
Even without a traditional cycle, tracking symptoms can be beneficial for your health and well-being. Instead of a cycle tracker, consider these methods:
-
Symptom Journal: A simple notebook where you record daily symptoms, their severity, and any related factors (e.g., stress levels, diet).
-
Mood Tracker Apps: Many apps are designed to track mood, energy levels, and sleep patterns. These can be adapted for post-hysterectomy symptom tracking.
-
Spreadsheet: Create a custom spreadsheet to track specific symptoms relevant to your individual experience.
-
Health Apps: Use a general health app to monitor sleep, activity levels, and diet, which can all impact symptom management.
When to See a Doctor
It’s always essential to consult with your doctor after a hysterectomy. Schedule regular check-ups to discuss any concerns and monitor your overall health. Seek medical advice if you experience:
- Severe pain
- Heavy bleeding (if cervix remains)
- Signs of infection (fever, redness, swelling)
- Difficulty urinating or bowel movements
- Significant emotional distress
Post-Hysterectomy Cycle Tracker FAQs
Here are some frequently asked questions about what to expect after a hysterectomy and the relevance of cycle tracking afterward.
Will I still have periods after a hysterectomy?
No, you will no longer have menstrual periods after a hysterectomy where the uterus is removed. Since the uterus is where menstruation occurs, its absence eliminates the possibility of periods.
Is there a cycle tracker for post-hysterectomy? What can I track?
While you won’t track menstrual cycles in the traditional sense, you can track other post-operative symptoms. This might include tracking mood changes, energy levels, sleep patterns, pain levels, and any hormone replacement therapy (HRT) side effects. Tracking these can help manage post-surgery well-being.
If my ovaries were removed, will I experience menopause symptoms?
Yes, if your ovaries were removed during the hysterectomy (oophorectomy), you will likely experience menopause symptoms. This is because the ovaries are the primary producers of estrogen and progesterone. Symptoms can include hot flashes, night sweats, vaginal dryness, and mood changes.
Even without a uterus, can I still experience cyclical symptoms?
Some women report experiencing cyclical symptoms even after a hysterectomy, especially if their ovaries were not removed. This could be due to hormonal fluctuations produced by the ovaries. If this is something you are experiencing, consider tracking these cyclical symptoms to see if you can identify the patterns.
So, while you won’t be tracking periods in the traditional sense, exploring what’s happening with your body after a hysterectomy is empowering. And when it comes to the question, is there a cycle tracker for post hysterectomy, remember that symptom tracking, self-care, and communication with your doctor are all valuable tools.