Basilar Tip Aneurysm: Saving Lives Through Early Detection
Understanding basilar tip aneurysm is crucial, and early detection can truly save lives. The brainstem, the life-sustaining structure affected by a basilar tip aneurysm, requires specialized care. Neurovascular surgeons possess the skills necessary to treat this condition effectively. Advancements in diagnostic imaging, particularly with tools like cerebral angiography, offer improved visualization that aids in the timely identification of a basilar tip aneurysm, allowing for prompt intervention to improve patient outcomes.
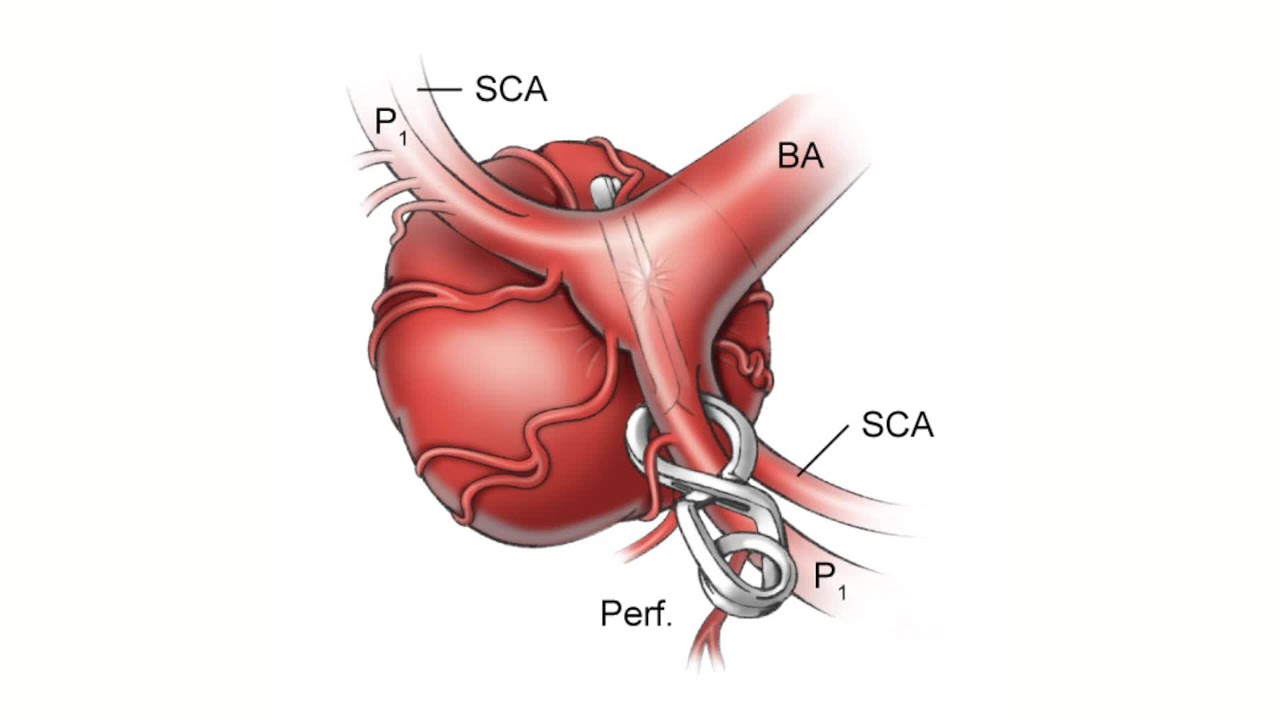
Image taken from the YouTube channel Barrow Neurological Institute , from the video titled Episode 2: Beginning to Climb – Giant Basilar Tip Aneurysm Clipping .
The human brain, an intricate network of vessels and tissues, is the control center of our existence. Within this complex organ, the basilar artery plays a crucial role, supplying blood to vital areas that govern essential functions. However, at the point where this artery bifurcates, or splits, lies a potential vulnerability: the basilar tip aneurysm.
These aneurysms, characterized by a bulging or weakening in the artery wall, pose a significant threat due to their location and the potential for rupture, leading to severe neurological damage or even death. This article aims to shed light on the nature of basilar tip aneurysms, emphasizing the importance of early detection and intervention.
Understanding Basilar Tip Aneurysms
A basilar tip aneurysm is a specific type of brain aneurysm that occurs at the bifurcation of the basilar artery. The basilar artery is located at the base of the brain, supplying blood to the brainstem, cerebellum, and occipital lobes. These areas are responsible for critical functions such as breathing, balance, coordination, and vision.
When an aneurysm forms at this location, it can disrupt blood flow and, if it ruptures, cause a subarachnoid hemorrhage (SAH). SAH is a life-threatening condition that requires immediate medical attention.
The Importance of Early Detection and Timely Intervention
Early detection of basilar tip aneurysms is paramount for improving patient outcomes. Unfortunately, these aneurysms often remain asymptomatic until they rupture, making proactive screening and awareness crucial.
With timely diagnosis, interventions can be implemented to prevent rupture and subsequent SAH. These interventions range from minimally invasive endovascular procedures to open surgical techniques, each tailored to the specific characteristics of the aneurysm and the overall health of the patient.
Article Purpose and Scope
This article serves as an informative resource for understanding basilar tip aneurysms. We will explore the key aspects of this condition, from its definition and location to its potential causes and risk factors. Our goal is to provide insights into the diagnostic process, treatment options, and long-term management strategies.
By equipping readers with this knowledge, we hope to empower them to make informed decisions about their brain health and to advocate for proactive care.
Addressing the Devastating Outcome of Subarachnoid Hemorrhage
One of the most feared consequences of a ruptured basilar tip aneurysm is subarachnoid hemorrhage (SAH). SAH occurs when blood leaks into the space surrounding the brain, causing a sudden and severe headache, often described as the "worst headache of my life."
Other symptoms may include stiff neck, loss of consciousness, seizures, and neurological deficits. The mortality rate associated with SAH is significant, and even with prompt treatment, many survivors experience long-term disabilities.
Raising Awareness and Advocating for Proactive Brain Health Management
Ultimately, the goal of this article is to raise awareness about basilar tip aneurysms and to advocate for proactive brain health management. We believe that knowledge is power, and by understanding the risks and potential consequences of this condition, individuals can take steps to protect themselves and their loved ones.
This includes discussing risk factors with healthcare providers, undergoing appropriate screening when indicated, and adopting lifestyle choices that promote overall brain health. Together, we can work towards a future where basilar tip aneurysms are detected early, treated effectively, and their devastating consequences are minimized.
The previous section touched upon the urgency surrounding basilar tip aneurysms. But before diving into detection and intervention, it’s crucial to build a solid foundation of understanding. What exactly is a basilar tip aneurysm, and why does its location make it so dangerous?
Understanding Basilar Tip Aneurysms: Location, Function, and Risks
A basilar tip aneurysm is, at its core, a localized weakening in the wall of the basilar artery. This weakening leads to a bulge or ballooning, much like a weak spot in a tire.
But what sets it apart is where this occurs – at the very tip of the basilar artery, where it splits, or bifurcates, into the posterior cerebral arteries.
The Basilar Artery: A Vital Highway
To fully grasp the significance, we need to understand the role of the basilar artery itself.
Imagine it as a major highway at the base of your brain. This artery is responsible for supplying blood to the brainstem, cerebellum, and occipital lobes.
These aren’t just any regions; they control functions absolutely essential for life.
The brainstem governs breathing, heart rate, and consciousness. The cerebellum is responsible for balance, coordination, and motor control.
And the occipital lobes are dedicated to visual processing.
Damage to any of these areas can have devastating consequences, underscoring the critical role the basilar artery plays in maintaining overall neurological function.
Why the Bifurcation Matters
The basilar artery’s bifurcation point is inherently vulnerable. The splitting of the artery creates a point of increased hemodynamic stress – essentially, more force is exerted on the artery walls at this location.
Over time, this increased stress can contribute to the weakening of the arterial wall, making it susceptible to aneurysm formation. This is similar to how a balloon is more likely to burst at its thinnest point.
Unraveling the Causes and Risks
While the exact cause of basilar tip aneurysms isn’t always clear, several factors are known to increase the risk of developing them.
These can broadly be categorized as genetic predispositions and acquired conditions.
Genetic Predispositions
Some individuals are born with inherent weaknesses in their blood vessel walls, making them more prone to aneurysm formation. Certain genetic conditions, such as Ehlers-Danlos syndrome and polycystic kidney disease, are associated with an increased risk of aneurysms.
A family history of aneurysms, even without a specific genetic diagnosis, can also elevate an individual’s risk.
Acquired Conditions and Lifestyle Factors
-
Hypertension (High Blood Pressure): Chronically elevated blood pressure puts extra stress on artery walls, increasing the risk of weakening and aneurysm formation.
-
Smoking: Smoking damages blood vessels, making them more brittle and susceptible to aneurysm development and rupture.
-
Atherosclerosis: The buildup of plaque in arteries can weaken the artery walls and disrupt blood flow, contributing to aneurysm formation.
-
Age: The risk of aneurysms generally increases with age as blood vessels naturally weaken over time.
-
Substance Abuse: Cocaine and other drugs can significantly increase blood pressure and damage blood vessels, raising the risk of aneurysm formation and rupture.
Understanding these risk factors is crucial for assessing individual susceptibility and implementing proactive strategies for prevention and early detection. Recognizing the connection between these factors and overall brain health emphasizes the importance of a holistic approach to well-being.
The previous section touched upon the urgency surrounding basilar tip aneurysms. But before diving into detection and intervention, it’s crucial to build a solid foundation of understanding. What exactly is a basilar tip aneurysm, and why does its location make it so dangerous?
The Silent Threat: Recognizing Subtle Symptoms and Risk Factors
One of the most insidious aspects of brain aneurysms, particularly unruptured ones, is their frequently asymptomatic nature.
Many individuals live their lives completely unaware that they harbor a potentially life-threatening weakness in a blood vessel within their brain. This "silent threat" underscores the critical need for awareness and proactive screening, especially for those with identified risk factors.
The Absence of Warning: Why Aneurysms Can Remain Hidden
The reason aneurysms often go unnoticed is that they typically don’t disrupt normal brain function until they either grow large enough to press on surrounding tissues or, more alarmingly, rupture.
Before either of these events occurs, the aneurysm may remain clinically silent, casting a shadow of potential danger without any outward signs.
Deciphering the Whispers: Subtle Symptoms That May Signal Danger
Although many aneurysms are silent, some can manifest with subtle symptoms.
Recognizing these potential warning signs, however faint, can be life-saving.
It’s essential to remember that these symptoms can be vague and may be attributed to other, less serious conditions, making accurate and timely diagnosis challenging.
Headaches: Atypical Pain That Demands Attention
One potential symptom is a change in the pattern or severity of headaches. A sudden, unusually severe headache – often described as a "thunderclap headache" – is a major red flag and warrants immediate medical attention.
However, more subtle, persistent headaches that are different from usual headaches should also be evaluated.
Visual Disturbances: When Sight Becomes a Concern
Aneurysms can sometimes press on cranial nerves, particularly those controlling eye movement and vision.
This pressure can lead to double vision (diplopia), blurred vision, drooping of the eyelid (ptosis), or other visual disturbances. Any new or unexplained changes in vision should prompt a visit to a healthcare professional.
Cranial Nerve Palsies: Neurological Deficits
In some cases, an aneurysm can directly compress a cranial nerve, leading to a cranial nerve palsy. This can result in a variety of symptoms depending on the nerve affected, including facial weakness, difficulty swallowing, or changes in taste.
It is important to note that the absence of these symptoms does not guarantee the absence of an aneurysm.
Understanding the Landscape: Navigating Risk Factors
While the exact cause of brain aneurysms is not fully understood, several risk factors have been identified that increase an individual’s likelihood of developing one. Understanding these factors is crucial for assessing personal risk and making informed decisions about preventative measures.
Genetic Predisposition: The Role of Family History
A family history of brain aneurysms or certain genetic conditions, such as polycystic kidney disease or Ehlers-Danlos syndrome, significantly increases the risk.
Individuals with a strong family history should discuss screening options with their healthcare provider.
Lifestyle Choices: Modifiable Factors
Certain lifestyle choices can also contribute to aneurysm development and rupture.
Smoking is a well-established risk factor, as it damages blood vessel walls. High blood pressure puts excessive stress on arteries, increasing the likelihood of aneurysm formation and rupture.
Excessive alcohol consumption and drug abuse can also weaken blood vessels.
Pre-existing Conditions: Underlying Health Issues
Certain pre-existing conditions can increase the risk of developing brain aneurysms.
These include connective tissue disorders, which weaken blood vessel walls, and conditions that cause inflammation of the arteries. Managing these underlying health issues can help mitigate the risk.
Ultimately, recognizing the silent threat of unruptured brain aneurysms requires a combination of awareness, vigilance, and proactive health management. By understanding the potential symptoms and risk factors, individuals can empower themselves to seek timely medical attention and make informed decisions about their brain health.
The subtle clues and silent progression of basilar tip aneurysms can be deceptive. While understanding the risk factors and potential symptoms forms a crucial first line of defense, it’s the timely recognition of these factors and the subsequent pursuit of early detection that truly shift the odds in a patient’s favor.
The Urgency of Early Detection: Why Time is of the Essence
In the realm of basilar tip aneurysms, time is not merely a factor; it is the very currency of survival and well-being. The insidious nature of these aneurysms, often lurking undetected until a catastrophic rupture occurs, underscores the critical importance of early detection. Swift diagnosis and intervention can drastically alter the course of this condition, transforming a potentially devastating outcome into a manageable one.
The Ticking Clock: Mitigating the Risk of Rupture
The primary danger associated with basilar tip aneurysms is the risk of rupture, leading to a subarachnoid hemorrhage (SAH). SAH is a life-threatening condition with significant morbidity and mortality rates. Every moment an aneurysm remains undetected, the risk of rupture persists, casting a shadow over the individual’s future.
Early detection allows for proactive management strategies aimed at stabilizing the aneurysm and preventing rupture. This can involve lifestyle modifications, medication to control blood pressure, or, in many cases, interventional procedures to secure the aneurysm. By identifying and addressing the aneurysm before it ruptures, we seize control of the narrative, significantly reducing the likelihood of SAH and its dire consequences.
Proactive Management: Averting Crisis Through Early Diagnosis
Early diagnosis is not just about preventing rupture; it’s about empowering proactive management. Once an aneurysm is identified, a team of specialists – neurosurgeons, neurologists, and interventional neuroradiologists – can collaborate to develop a personalized treatment plan.
This plan may involve careful monitoring with regular imaging to assess the aneurysm’s growth and stability. Or, it may entail intervention, such as endovascular coiling or surgical clipping, to eliminate the risk of rupture altogether. The ability to make these informed decisions before a crisis strikes is invaluable.
Awareness and Vigilance: The Cornerstones of Early Detection
The cornerstone of early detection is, quite simply, awareness. Knowing the risk factors associated with basilar tip aneurysms – family history, smoking, high blood pressure, certain genetic conditions – is the first step. If you possess any of these risk factors, it is essential to engage in open and honest conversations with your healthcare provider.
Regular check-ups, including neurological examinations, can help identify potential warning signs or prompt further investigation. For individuals with a strong family history or other significant risk factors, screening with advanced imaging techniques, such as MRA or CTA, may be warranted, even in the absence of symptoms. Vigilance and proactive engagement with your healthcare team are key to safeguarding your brain health.
The proactive measures discussed are invaluable in mitigating risk. However, when symptoms do arise, or when risk factors necessitate further investigation, the journey towards diagnosis begins.
Diagnosis: Advanced Imaging Techniques for Identifying Aneurysms
The diagnosis of basilar tip aneurysms is a multi-faceted process, demanding a combination of careful clinical evaluation and cutting-edge imaging technologies. It is a journey of discovery, where medical expertise and technological innovation converge to unveil the hidden threat.
The process typically commences with a thorough neurological examination, where a physician assesses the patient’s neurological function, looking for signs and symptoms that might indicate the presence of an aneurysm.
This examination is crucial, as it provides the initial clues and guides the subsequent diagnostic steps.
The Role of Imaging Techniques
While a neurological examination can raise suspicion, the definitive diagnosis of a basilar tip aneurysm relies on advanced imaging techniques. These techniques allow physicians to visualize the intricate network of blood vessels within the brain and identify any abnormalities, such as aneurysms.
Cerebral angiography, computed tomography angiography (CTA), and magnetic resonance angiography (MRA) are the primary tools used in this diagnostic process. Each technique offers unique advantages and provides complementary information, ensuring a comprehensive assessment.
Cerebral Angiography: The Gold Standard
Cerebral angiography, also known as digital subtraction angiography (DSA), is often considered the gold standard for visualizing blood vessels in the brain.
This invasive procedure involves inserting a catheter into an artery, typically in the groin, and guiding it to the blood vessels in the brain. A contrast dye is then injected, and X-ray images are taken, providing a detailed view of the cerebral vasculature.
Cerebral angiography offers exceptional resolution, allowing physicians to visualize even small aneurysms and assess their characteristics with great precision.
However, due to its invasive nature, it is typically reserved for cases where other imaging techniques are inconclusive or when intervention is planned.
Computed Tomography Angiography (CTA): A Rapid and Non-Invasive Approach
Computed tomography angiography (CTA) is a non-invasive imaging technique that uses computed tomography (CT) to visualize blood vessels. During a CTA scan, a contrast dye is injected into a vein, and a series of X-ray images are taken as the dye travels through the blood vessels.
These images are then processed by a computer to create a three-dimensional reconstruction of the cerebral vasculature.
CTA is a rapid and readily available imaging technique, making it particularly useful in emergency situations, such as the evaluation of patients with suspected subarachnoid hemorrhage. It provides a good overview of the blood vessels and can detect most aneurysms.
Magnetic Resonance Angiography (MRA): Detailed Imaging Without Radiation
Magnetic resonance angiography (MRA) is another non-invasive imaging technique that uses magnetic resonance imaging (MRI) to visualize blood vessels.
MRA does not involve the use of ionizing radiation, making it a safe option for patients who require repeated imaging.
MRA provides detailed images of the cerebral vasculature and can be particularly useful for evaluating aneurysms located in the posterior circulation, including basilar tip aneurysms. It excels in visualizing the relationship between the aneurysm and surrounding brain structures.
Determining Size, Shape, and Location
The information gleaned from these advanced imaging techniques is crucial for determining the optimal management strategy for basilar tip aneurysms. The size, shape, and precise location of the aneurysm are all critical factors that influence the risk of rupture and the feasibility of different treatment options.
Imaging helps the specialists to understand the aneurysm’s morphology (shape) and its relation to adjacent vessels and brain tissue, which is pivotal in pre-surgical planning and risk assessment.
By accurately characterizing the aneurysm, physicians can make informed decisions about whether to pursue conservative management or interventional treatment.
The imaging techniques we’ve explored play a crucial role in identifying basilar tip aneurysms, providing a detailed roadmap of these vascular anomalies. But diagnosis is only the first step. Once an aneurysm is detected, the focus shifts to determining the most appropriate course of action to prevent rupture and safeguard the patient’s neurological health.
Treatment Options: Navigating the Path to Prevention and Management
The management of basilar tip aneurysms is a complex undertaking, requiring careful consideration of various treatment options. The primary goal is to prevent rupture and subsequent subarachnoid hemorrhage, a potentially devastating event. Fortunately, advancements in medical technology have provided us with two main approaches: endovascular coiling and surgical clipping.
Endovascular Coiling: A Minimally Invasive Approach
Endovascular coiling has revolutionized the treatment of many brain aneurysms, offering a less invasive alternative to traditional surgery. The procedure involves threading a catheter through an artery, typically in the groin, and guiding it to the site of the aneurysm in the brain.
Once the catheter is positioned within the aneurysm sac, tiny platinum coils are deployed. These coils conform to the shape of the aneurysm, filling the space and blocking blood flow into the aneurysm. Over time, this promotes clotting within the aneurysm, effectively sealing it off from the parent artery.
The beauty of endovascular coiling lies in its minimally invasive nature. It typically requires a shorter hospital stay, involves less pain, and results in a quicker recovery compared to surgical clipping. However, it may not be suitable for all types of aneurysms, and there is a risk of recurrence, requiring further treatment.
Surgical Clipping: A Time-Tested Technique
Surgical clipping, also known as open surgery, is a more traditional approach to treating basilar tip aneurysms. This involves a craniotomy, where a portion of the skull is removed to access the brain.
Under microscopic visualization, the neurosurgeon carefully identifies the aneurysm and its relationship to the surrounding blood vessels and brain tissue. A small metal clip is then placed at the neck or base of the aneurysm, effectively isolating it from the normal circulation.
This prevents blood from entering the aneurysm, eliminating the risk of rupture.
Surgical clipping offers a durable, long-term solution for many aneurysms. However, it is a more invasive procedure than endovascular coiling, with a longer recovery period and a higher risk of complications.
Choosing the Right Approach: A Collaborative Decision
The decision of whether to pursue endovascular coiling or surgical clipping is not taken lightly. It requires a multidisciplinary approach, involving neurosurgeons, neurologists, and interventional neuroradiologists.
Several factors are carefully considered, including:
-
Aneurysm Size, Shape, and Location: The specific characteristics of the aneurysm, such as its size, shape, and precise location on the basilar artery, play a crucial role in determining the most appropriate treatment. Some aneurysms are more amenable to coiling, while others are better suited for clipping.
-
Patient’s Overall Health: The patient’s general health, age, and any pre-existing medical conditions are taken into account. Patients with significant health problems may be better candidates for the less invasive coiling procedure.
-
Surgeon’s Expertise: The experience and expertise of the neurosurgeon and interventional neuroradiologist are also important considerations. Some surgeons may have more experience with one technique over the other.
-
Potential Risks and Benefits: A thorough discussion of the potential risks and benefits of each procedure is essential to ensure that the patient is fully informed and can make an informed decision.
-
Durability and Long-Term Outcomes: The long-term effectiveness of each procedure is also considered. While surgical clipping offers a more definitive, long-term solution, endovascular coiling may require further treatments in the future.
It is important to remember that there is no one-size-fits-all approach to treating basilar tip aneurysms. The optimal treatment strategy is tailored to the individual patient and the specific characteristics of their aneurysm. This collaborative, patient-centered approach ensures that the most appropriate and effective treatment is chosen, maximizing the chances of a positive outcome.
The imaging techniques we’ve explored play a crucial role in identifying basilar tip aneurysms, providing a detailed roadmap of these vascular anomalies. But diagnosis is only the first step. Once an aneurysm is detected, the focus shifts to determining the most appropriate course of action to prevent rupture and safeguard the patient’s neurological health.
Life After Treatment: Charting the Course of Recovery and Long-Term Well-being
Undergoing treatment for a basilar tip aneurysm marks the beginning of a new chapter, one focused on recovery, adaptation, and proactive management. The journey doesn’t end with the successful coiling or clipping of the aneurysm; instead, it transitions to a phase that demands vigilance, patience, and a commitment to long-term neurological health.
The Initial Recovery Period: Navigating Potential Challenges
The immediate aftermath of aneurysm treatment can present a variety of challenges, both physical and emotional. Depending on the treatment approach (endovascular coiling or surgical clipping), patients may experience pain, fatigue, and temporary neurological deficits.
It’s crucial to understand that these initial symptoms are often a normal part of the healing process. However, any new or worsening symptoms should be promptly reported to the medical team.
Common challenges during this period include:
- Pain management: Post-operative pain is common and is usually managed with medication.
- Fatigue: Recovering from any medical procedure, especially one involving the brain, can be physically and mentally exhausting.
- Headaches: These can persist for some time after treatment and may require specific management strategies.
- Neurological deficits: Some patients may experience temporary weakness, speech difficulties, or vision changes. These often improve with time and rehabilitation.
The Indispensable Role of Rehabilitation
Rehabilitation plays a vital role in optimizing recovery and regaining lost function. A tailored rehabilitation program, designed by specialists, can help patients overcome physical and cognitive challenges.
This may involve:
- Physical therapy: To improve strength, balance, and coordination.
- Occupational therapy: To regain skills needed for daily living activities.
- Speech therapy: To address speech, language, or swallowing difficulties.
- Cognitive rehabilitation: To improve memory, attention, and problem-solving skills.
Active participation in rehabilitation is crucial for achieving the best possible outcome.
The Importance of Ongoing Neurological Monitoring
Even after a successful procedure and initial recovery, ongoing monitoring is essential. Regular follow-up appointments with a neurologist are crucial for detecting any potential complications and ensuring long-term stability.
These appointments typically involve neurological examinations, imaging studies (such as MRA or CTA), and assessments of cognitive function.
Lifestyle Modifications: Nurturing Long-Term Brain Health
Beyond medical interventions and rehabilitation, adopting a healthy lifestyle is paramount for long-term well-being.
This includes:
- Managing blood pressure: High blood pressure is a significant risk factor for aneurysm formation and rupture. Maintain a healthy blood pressure through diet, exercise, and medication, if necessary.
- Quitting smoking: Smoking damages blood vessels and increases the risk of aneurysm development.
- Maintaining a healthy weight: Obesity can contribute to high blood pressure and other risk factors.
- Eating a balanced diet: A diet rich in fruits, vegetables, and whole grains supports overall health and vascular function.
- Regular exercise: Physical activity improves cardiovascular health and reduces the risk of stroke.
- Limiting alcohol consumption: Excessive alcohol intake can increase blood pressure and may contribute to aneurysm rupture.
Addressing Potential Complications
While treatment aims to eliminate the risk of rupture, potential complications can still arise. These may include:
- Aneurysm recurrence: In rare cases, the aneurysm may regrow or a new aneurysm may form.
- Hydrocephalus: A buildup of fluid in the brain.
- Vasospasm: Narrowing of blood vessels in the brain.
- Seizures: These can occur as a result of brain injury.
Prompt identification and management of these complications are critical. It’s important to maintain open communication with your medical team and report any new or concerning symptoms.
Emotional and Psychological Well-being
The experience of having a brain aneurysm can be emotionally challenging. It’s essential to acknowledge and address the psychological impact of diagnosis and treatment.
Anxiety, depression, and fear are common emotions. Seeking support from therapists, counselors, or support groups can be invaluable in coping with these challenges and fostering emotional resilience.
Living a Full and Meaningful Life
Life after treatment for a basilar tip aneurysm is about more than just managing physical health; it’s about reclaiming your life and pursuing your passions. With proactive management, a healthy lifestyle, and a strong support system, individuals can thrive and live full, meaningful lives. Remember to prioritize self-care, engage in activities that bring you joy, and maintain strong connections with loved ones.
Basilar Tip Aneurysm FAQs
Here are some frequently asked questions about basilar tip aneurysms and their early detection.
What exactly is a basilar tip aneurysm?
A basilar tip aneurysm is a bulge or ballooning in the wall of the basilar artery, specifically at its tip where it divides into other important brain arteries. This weakening in the artery wall can lead to rupture and potentially life-threatening bleeding in the brain.
Why is early detection so crucial for basilar tip aneurysms?
Early detection allows for timely intervention before the aneurysm ruptures. Treatment options like coiling or clipping can prevent a potentially devastating hemorrhage, significantly improving patient outcomes and chances of survival after basilar tip aneurysm detection.
What are some common symptoms of a basilar tip aneurysm before it ruptures?
Unfortunately, many basilar tip aneurysms are asymptomatic until they rupture. However, larger aneurysms may sometimes cause symptoms like double vision, headache, facial pain, or numbness due to pressure on surrounding brain structures. If you experience persistent, unexplained symptoms, it’s essential to seek medical attention.
How are basilar tip aneurysms typically diagnosed?
Diagnosis usually involves imaging techniques like CT angiography (CTA) or MR angiography (MRA). These scans can visualize the blood vessels in the brain and identify the presence, size, and location of the basilar tip aneurysm, allowing doctors to formulate the best treatment plan.
So, while a basilar tip aneurysm sounds scary, remember knowledge is power! Hopefully, this has given you some helpful insights and a better understanding. Stay vigilant about your health, and don’t hesitate to talk to your doctor if you have any concerns.